Cholangitis, also known as inflammation of the bile ducts, is a condition that can significantly impact liver function and overall health. It occurs when the bile ducts, which carry digestive fluids from the liver to the small intestine, become infected or inflamed. Understanding this condition is essential for early detection, effective treatment, and prevention of potential complications. This article provides a comprehensive overview of cholangitis, including its causes, symptoms, diagnostic methods, treatment options, and strategies for maintaining bile duct health. Whether you are a healthcare professional or an individual seeking knowledge, this guide aims to present clear and detailed information about cholangitis.
Understanding Cholangitis: An Overview of the Condition
Cholangitis is primarily characterized by inflammation and infection of the bile ducts, which are part of the biliary system responsible for transporting bile. Bile is a digestive fluid produced by the liver that helps break down fats in the small intestine. When the bile ducts become obstructed or infected, bile flow is hindered, leading to a build-up of bile and potential damage to liver tissue. The condition can manifest acutely, with rapid onset and severe symptoms, or develop chronically, resulting in long-term liver issues. The most common form is ascending cholangitis, where bacteria ascend from the intestine into the bile ducts, causing infection.
The anatomy of the biliary system includes the intrahepatic bile ducts within the liver and the extrahepatic ducts that extend outside the liver, eventually draining into the small intestine. Any disruption or blockage in these pathways can predispose individuals to cholangitis. The condition is more prevalent in adults, especially those with pre-existing liver or biliary diseases. It can affect individuals of all ages, although certain groups such as the elderly or those with biliary stones are at higher risk. Recognizing the importance of prompt diagnosis and management is crucial to prevent serious health consequences.
Cholangitis often presents as a medical emergency, particularly in its acute form, requiring immediate attention. The inflammation can lead to systemic infection, sepsis, and even multi-organ failure if untreated. Chronic cholangitis may contribute to progressive liver damage, fibrosis, or cirrhosis over time. Understanding the underlying mechanisms and recognizing early signs are vital components of effective healthcare. Advances in medical imaging and laboratory testing have improved the ability to diagnose and treat this condition effectively, reducing the risk of severe outcomes.
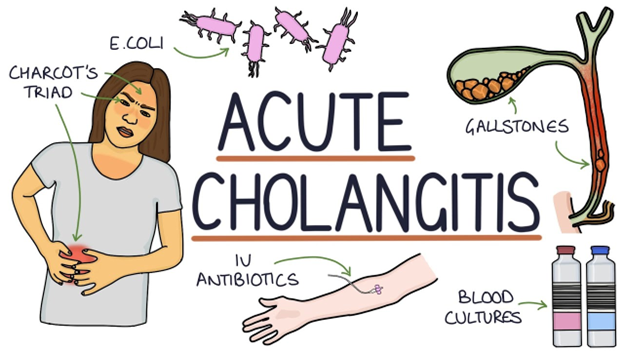
The pathophysiology of cholangitis involves bacterial infection, often caused by bacteria such as Escherichia coli, Klebsiella, or Enterococcus, which ascend from the gastrointestinal tract. The infection causes swelling and inflammation within the bile ducts, leading to symptoms like pain, fever, and jaundice. The presence of stones, strictures, or tumors can obstruct bile flow and serve as a nidus for infection. Understanding these mechanisms helps healthcare providers tailor treatment strategies and address the root causes of the disease.
In summary, cholangitis is a complex condition involving inflammation and infection of the bile ducts that can have serious health implications if not properly managed. Its diverse causes and presentations necessitate a comprehensive approach to diagnosis and treatment. Awareness and early intervention are key to improving outcomes and maintaining liver health over the long term.
Causes and Risk Factors Associated with Cholangitis
Cholangitis is primarily caused by infection, often resulting from an obstruction in the bile ducts that allows bacteria to ascend and infect the biliary system. The most common cause of obstruction is the presence of gallstones, which can block the bile ducts and create a conducive environment for bacterial growth. Other causes include strictures—narrowing of the ducts due to inflammation, scarring, or tumors—that impede normal bile flow, increasing the risk of infection.
Tumors, such as cholangiocarcinoma or pancreatic cancer, can also cause obstructions in the biliary system, leading to cholangitis. Additionally, congenital anomalies, such as biliary atresia or ductal malformations, can predispose individuals to develop this condition. In some cases, prior surgical procedures, especially those involving the biliary or hepatic regions, may result in scar tissue or strictures that block bile flow and heighten infection risk.
Risk factors for cholangitis extend beyond anatomical issues. Conditions that impair immune function, such as HIV/AIDS or diabetes mellitus, can increase susceptibility to infections, including those affecting the bile ducts. Age is also a factor; older adults are more likely to develop biliary obstructions and subsequent infections due to degenerative changes and comorbidities. Furthermore, individuals with a history of recurrent biliary stones or previous episodes of cholangitis are at heightened risk of recurrence.
Lifestyle factors may influence the risk of developing cholangitis as well. Poor diet, obesity, and sedentary habits can contribute to the formation of gallstones, a common cause of biliary obstruction. Additionally, certain infections or parasitic infestations, such as liver flukes, are prevalent in specific regions and can lead to chronic inflammation and increased risk of cholangitis. Recognizing these risk factors enables clinicians to identify high-risk populations and implement preventive strategies.
Overall, cholangitis arises from a combination of anatomical, infectious, and systemic factors. Understanding these causes and risk factors is essential for early detection, targeted prevention, and effective management. Addressing underlying issues such as gallstone disease or strictures can significantly reduce the incidence and severity of cholangitis episodes.
Common Symptoms and Signs of Bile Duct Infection
The clinical presentation of cholangitis can vary depending on whether the condition is acute or chronic, but certain symptoms are commonly observed across cases. In acute cholangitis, patients often experience a sudden onset of right upper quadrant abdominal pain, which may radiate to the back or shoulder. This pain is typically persistent and may worsen with movement or deep breathing. Alongside pain, fever and chills are hallmark signs of infection, indicating systemic inflammatory response.
Jaundice, characterized by yellowing of the skin and sclerae, is another prominent symptom resulting from the blockage of bile flow. When bile cannot reach the intestine, bilirubin accumulates in the bloodstream, leading to the characteristic discoloration. Patients may also report dark urine and pale stools, which are indicative of disrupted bile excretion. In some cases, symptoms such as nausea, vomiting, and general malaise accompany the primary signs of cholangitis.
In chronic or less severe cases, symptoms may be more subtle or intermittent, including mild abdominal discomfort, fatigue, and occasional episodes of jaundice. These patients might not exhibit the classic signs of infection but may experience recurrent episodes of biliary pain or discomfort. Chronic cholangitis can also lead to progressive liver damage, which might manifest as hepatomegaly or signs of cirrhosis in advanced stages.
Laboratory findings often support the clinical picture, with elevated liver enzymes such as alkaline phosphatase, gamma-glutamyl transferase (GGT), and bilirubin levels. Leukocytosis, or increased white blood cell count, is common in infections, reflecting systemic inflammation. Blood cultures may sometimes identify causative bacteria, especially in severe cases. Recognizing these signs and symptoms promptly is essential for initiating appropriate diagnostic and therapeutic interventions.
The presentation of cholangitis can sometimes mimic other abdominal or hepatic conditions, making clinical suspicion crucial. Rapid recognition of symptoms, particularly in individuals with risk factors like gallstones or prior biliary surgery, can facilitate timely diagnosis and prevent complications. Patients experiencing these symptoms should seek medical evaluation to determine the underlying cause and receive appropriate care.
Diagnostic Procedures Used to Detect Cholangitis
Diagnosing cholangitis involves a combination of clinical evaluation, laboratory tests, and imaging studies. The initial assessment begins with a detailed medical history and physical examination focusing on symptoms such as abdominal pain, jaundice, and fever. Laboratory tests play a critical role in supporting the diagnosis; blood tests often reveal elevated liver function tests, including alkaline phosphatase, GGT, and bilirubin, alongside increased white blood cell counts indicative of infection.
Blood cultures are also performed to identify the causative bacteria, especially in severe or systemic cases. These cultures help guide antibiotic therapy by pinpointing specific pathogens. In addition, tests like liver function panels provide insights into the extent of liver involvement and bile obstruction. Sometimes, serologic tests are conducted to rule out other underlying conditions or parasitic infections that could contribute to biliary inflammation.
Imaging studies are indispensable for visualizing the biliary system and confirming the presence of obstructions or structural abnormalities. Ultrasonography is often the first-line imaging modality due to its availability, safety, and ability to detect gallstones, biliary dilation, or strictures. It can also identify other potential causes of biliary obstruction, such as tumors or cysts. When ultrasound findings are inconclusive or more detailed visualization is needed, further imaging techniques are employed.
Endoscopic procedures, such as endoscopic retrograde cholangiopancreatography (ERCP), serve both diagnostic and therapeutic purposes. ERCP allows direct visualization of the bile ducts, identification of stones or strictures, and the ability to remove obstructions or obtain tissue biopsies. Magnetic resonance cholangiopancreatography (MRCP) is a non-invasive imaging technique that provides detailed images of the biliary and pancreatic ducts without the need for contrast injection, making it suitable for initial assessment or follow-up.
Overall, a multidisciplinary approach combining clinical assessment, laboratory testing, and advanced imaging techniques is essential for accurate diagnosis of cholangitis. Early detection facilitates prompt management, reduces complications, and improves patient outcomes by targeting the underlying causes of bile duct inflammation.
The Role of Imaging Techniques in Cholangitis Diagnosis
Imaging techniques are vital tools in the diagnosis and management of cholangitis, providing detailed visualization of the biliary system to identify obstructions, strictures, stones, or tumors. Ultrasonography is typically the first imaging modality used due to its accessibility, safety, and ability to detect common causes like gallstones and bile duct dilation. It can reveal the presence of sludge, dilated intrahepatic or extrahepatic ducts, and