Choriocarcinoma is a rare but aggressive form of cancer that originates from trophoblastic tissue, which is involved in pregnancy. Despite its rarity, understanding this disease is crucial because of its potential severity and the importance of early diagnosis for effective treatment. This article provides a comprehensive overview of choriocarcinoma, including its causes, symptoms, diagnostic methods, treatment options, and ongoing research. By exploring these aspects, patients, healthcare providers, and caregivers can better recognize, manage, and support those affected by this condition. The goal is to shed light on this complex disease and emphasize the importance of awareness and timely intervention.
Understanding Choriocarcinoma: An Overview of the Disease
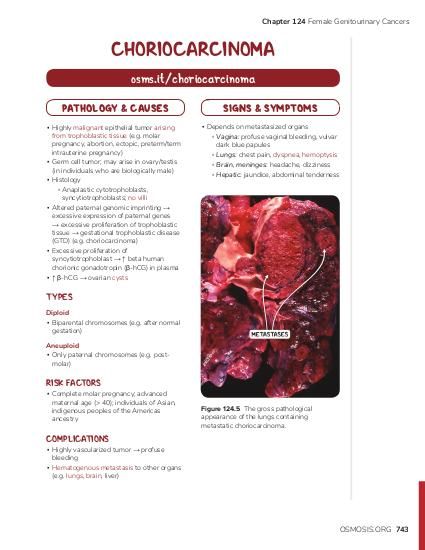
Choriocarcinoma is a malignant tumor that develops from trophoblastic cells, which are part of the tissue that forms the placenta during pregnancy. It can occur after any type of pregnancy, including full-term delivery, miscarriage, molar pregnancy, or ectopic pregnancy. The disease is characterized by rapid growth and a high propensity to spread to other parts of the body, such as the lungs, brain, liver, and vagina. Although it is a rare form of cancer, choriocarcinoma is considered highly treatable when diagnosed early. Its origin from placental tissue makes it unique among gynecologic cancers, and its behavior can differ significantly from other malignancies.
Choriocarcinoma is classified as a type of gestational trophoblastic disease (GTD), which encompasses a spectrum of placental tumors. It is distinguished by its malignant nature and ability to produce high levels of human chorionic gonadotropin (hCG), a hormone normally produced during pregnancy. The tumor’s rapid proliferation and tendency to metastasize often necessitate aggressive treatment strategies. Despite its potential for aggressive spread, the prognosis for choriocarcinoma has improved markedly with advances in diagnosis and therapy, especially when detected early.
The disease can manifest as either a standalone tumor or as part of a molar pregnancy, which is an abnormal growth of trophoblastic tissue within the uterus. Post-molar choriocarcinoma can develop weeks or months after the initial pregnancy event. Importantly, choriocarcinoma is not limited to women of reproductive age; although rare, cases have been reported in men, typically related to germ cell tumors. Understanding the biological behavior of choriocarcinoma is essential for developing effective treatment plans and improving patient outcomes.
The pathophysiology involves the malignant transformation of trophoblastic cells, leading to uncontrolled proliferation and invasion into surrounding tissues. These cells can produce large quantities of hCG, which serves as a biomarker for diagnosis and monitoring treatment response. The aggressive nature of choriocarcinoma underscores the importance of prompt recognition and intervention. Overall, while rare, choriocarcinoma’s rapid progression and potential for metastasis make it a significant concern in reproductive health and oncology.
Causes and Risk Factors Associated with Choriocarcinoma
The primary cause of choriocarcinoma is related to abnormal proliferation of trophoblastic tissue following pregnancy. It typically arises from gestational events, such as molar pregnancies, miscarriages, or full-term deliveries, where trophoblastic cells undergo malignant transformation. The exact molecular mechanisms behind this transformation are not entirely understood but involve genetic and epigenetic alterations that promote uncontrolled cell growth. In some cases, the disease develops without any identifiable antecedent pregnancy, although these instances are rare.
Certain factors can increase the risk of developing choriocarcinoma. A history of molar pregnancy is one of the most significant risk factors, especially if the molar pregnancy was complete rather than partial. Women with a prior history of gestational trophoblastic disease have a higher chance of recurrence and subsequent development of choriocarcinoma. Elevated levels of human chorionic gonadotropin (hCG) following pregnancy complications may also be indicative of underlying trophoblastic malignancy, although this is not a direct cause.
Genetic predispositions and environmental influences may also play roles in the development of choriocarcinoma. For example, certain genetic mutations could facilitate the malignant transformation of trophoblastic cells. Additionally, advanced maternal age has been associated with an increased risk, particularly in women over 35 years old. Socioeconomic factors and access to healthcare can influence early detection and management, indirectly affecting disease outcomes.
While the precise causes are linked to abnormal placental cell behavior, some theories suggest that immune system factors may contribute to the development of trophoblastic malignancies. However, no specific lifestyle or environmental exposures have been conclusively associated with increased risk. Overall, understanding the risk factors helps in identifying high-risk populations and underscores the importance of regular follow-up after pregnancy-related events to catch any abnormal growth early.
Preventive measures are limited due to the disease’s unpredictable nature, but awareness of risk factors can facilitate early detection. Women with a history of molar pregnancy or other trophoblastic diseases should undergo regular monitoring of hCG levels to detect any abnormal activity promptly. Continued research into the genetic and molecular basis of choriocarcinoma aims to identify potential preventive strategies and targeted therapies in the future.
Common Symptoms and Signs of Choriocarcinoma Development
Choriocarcinoma often presents with symptoms related to its rapid growth and metastatic spread. In women, one of the earliest indicators is abnormal vaginal bleeding, which may occur weeks or months after a pregnancy event such as a miscarriage, molar pregnancy, or delivery. The bleeding is typically irregular, heavy, or prolonged, prompting further investigation. Some women may notice pelvic pain or discomfort associated with the uterine mass or bleeding episodes.
Due to its aggressive nature and tendency to metastasize early, choriocarcinoma can also produce symptoms in distant organs. Pulmonary metastases are common, leading to symptoms such as cough, hemoptysis (coughing up blood), chest pain, or shortness of breath. When the disease spreads to the brain, neurological symptoms like headaches, seizures, or visual disturbances may occur. Liver involvement can cause abdominal pain, hepatomegaly, or signs of liver dysfunction.
In addition to physical symptoms, elevated levels of human chorionic gonadotropin (hCG) are a hallmark of the disease. Women with choriocarcinoma often have markedly high serum hCG levels, which can be detected through blood tests. These levels can sometimes be used to monitor disease progression or response to therapy. However, reliance solely on symptoms and hCG levels can be insufficient, emphasizing the importance of comprehensive diagnostic procedures.
Other signs may include systemic symptoms such as weight loss, fatigue, or malaise, especially in advanced stages. Some patients might experience anemia due to ongoing bleeding, or signs of metastasis like neurological deficits. Because symptoms can overlap with other gynecological or respiratory conditions, a high index of suspicion is necessary for timely diagnosis. Recognizing these signs early can significantly improve treatment outcomes and survival rates.
Overall, awareness of the diverse symptoms associated with choriocarcinoma is vital for early detection. Patients presenting with abnormal bleeding post-pregnancy or unexplained systemic symptoms should seek prompt medical evaluation. Healthcare providers must consider choriocarcinoma in differential diagnoses to facilitate early intervention and improve prognosis.
Diagnostic Procedures Used to Detect Choriocarcinoma
Diagnosing choriocarcinoma involves a combination of clinical assessment, laboratory tests, imaging studies, and tissue analysis. The initial step typically includes measuring serum human chorionic gonadotropin (hCG) levels, which are often markedly elevated in affected individuals. Persistent high hCG levels following pregnancy-related events raise suspicion of trophoblastic disease, prompting further investigation.
Pelvic ultrasound is a primary imaging modality used to evaluate the uterus. It can reveal a mass, irregular uterine contours, or the presence of a molar pregnancy. In cases where the uterus appears normal, additional imaging may be necessary to assess for metastasis. Chest X-rays or computed tomography (CT) scans are commonly employed to detect lung metastases, which are frequent in choriocarcinoma. Abdominal and brain imaging may also be performed if symptoms suggest spread to these regions.
In some cases, a biopsy of the uterine or metastatic lesion may be necessary for definitive diagnosis. However, because choriocarcinoma is highly vascular and prone to bleeding, biopsy procedures are approached with caution. Instead, the diagnosis is often made based on clinical presentation, elevated hCG levels, and characteristic imaging findings. Histopathological examination confirms the presence of malignant trophoblastic tissue, showing characteristic features such as hemorrhage, necrosis, and atypical trophoblastic cells.
Advanced diagnostic techniques include magnetic resonance imaging (MRI), which provides detailed information about soft tissue involvement and metastasis. Additionally, serial hCG measurements are crucial for monitoring treatment response and detecting recurrence. In some cases, molecular studies or genetic testing may be utilized to differentiate choriocarcinoma from other trophoblastic tumors or germ cell tumors.
Overall, a multidisciplinary approach combining laboratory, imaging, and histopathological assessments ensures accurate diagnosis. Early and precise detection is essential for initiating appropriate therapy and improving patient outcomes. Healthcare providers should maintain vigilance when evaluating women with abnormal bleeding or elevated hCG, especially if they have a history of pregnancy complications.
Staging and Classification of Choriocarcinoma
Staging and classification of choriocarcinoma are essential for determining the extent of disease spread and guiding treatment strategies. The FIGO (International Federation of Gynecology and Obstetrics) staging system is commonly used, which considers both the anatomical spread and serum hCG levels. This system classifies the disease from Stage I, confined to the uterus, to Stage IV, with distant metastases involving organs such as the lungs, brain, or liver.
Stage I indicates disease limited to the uterus, often associated with a better prognosis. Stage II involves local extension to the pelvis or adnexa but no distant metastasis. Stage III signifies spread to the lungs or other distant sites, while Stage IV indicates extensive metastasis to multiple organs. The FIGO scoring