Chronic Venous Insufficiency (CVI) is a common circulatory disorder that affects the veins in the legs, leading to improper blood flow back to the heart. Characterized by weakened vein walls and faulty valves, CVI can cause a range of symptoms and complications that impact quality of life. Understanding this condition is essential for early detection, effective management, and prevention. This article provides a comprehensive overview of CVI, exploring its causes, symptoms, diagnostic methods, treatment options, and strategies for living with the condition.
Understanding Chronic Venous Insufficiency: An Overview of the Condition
Chronic Venous Insufficiency is a long-term condition where the veins in the legs are unable to efficiently return blood to the heart. Normally, veins contain one-way valves that prevent blood from flowing backward as it moves upward against gravity. In CVI, these valves become damaged or weakened, leading to blood pooling in the lower extremities. Over time, this persistent venous hypertension causes changes in the vein walls and surrounding tissues. The condition is often progressive, worsening if left untreated, and can significantly impair mobility and comfort.
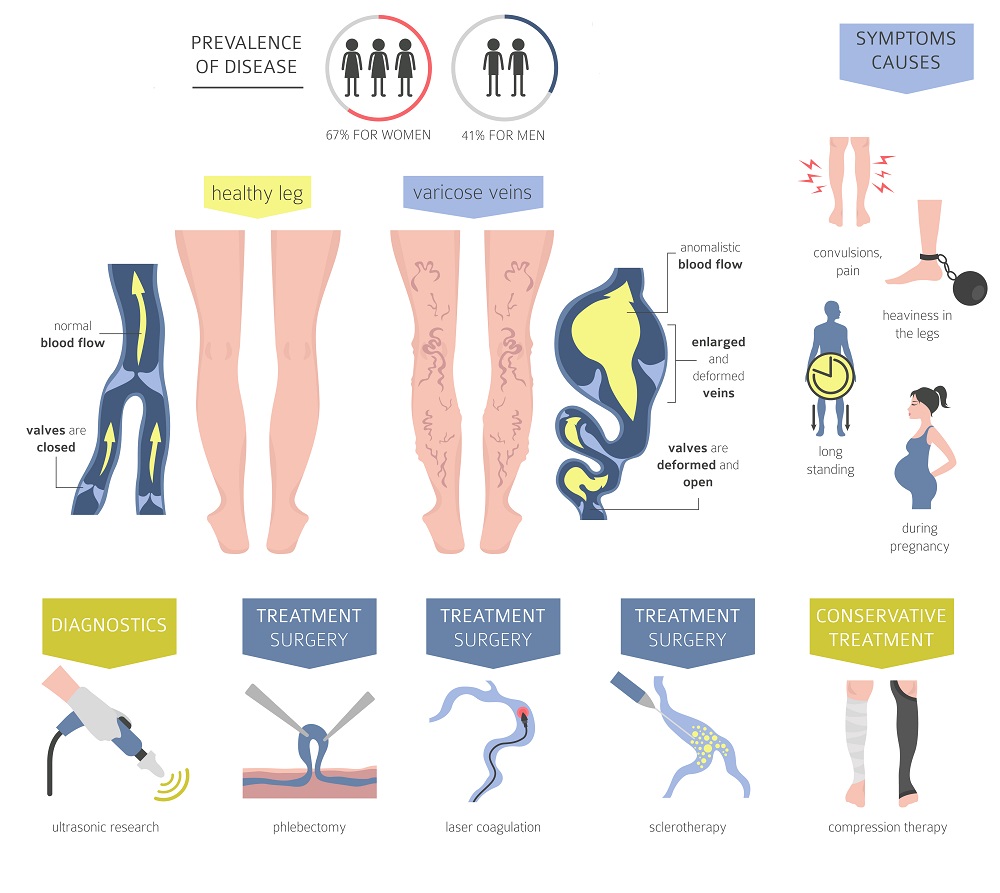
CVI affects a substantial portion of the adult population, especially as they age. It is more prevalent among individuals with a family history of venous disease, those who stand or sit for prolonged periods, and women, particularly during pregnancy. The chronic nature of CVI means that it often develops gradually, with symptoms becoming more noticeable over years. The condition not only causes physical discomfort but also poses risks for more severe complications such as skin ulcers and infections.
The pathophysiology of CVI involves increased venous pressure, inflammation, and venous wall remodeling. These changes can lead to varicose veins, skin discoloration, and tissue breakdown. The severity of the condition varies among individuals, with some experiencing mild symptoms, while others develop significant venous ulcers and skin changes. Understanding the underlying mechanisms helps in tailoring appropriate treatment strategies to prevent progression and manage symptoms.
Diagnosis of CVI is primarily clinical, supported by imaging studies such as duplex ultrasound, which assesses blood flow and vein structure. Early recognition and intervention are crucial to prevent irreversible tissue damage and improve patient outcomes. The condition is manageable through a combination of lifestyle modifications, medical treatments, and, in advanced cases, surgical interventions.
Overall, Chronic Venous Insufficiency is a complex vascular disorder with a significant impact on individuals’ health and wellbeing. Awareness of its nature and progression is key to effective management and improving quality of life for those affected.
Causes and Risk Factors Associated with Chronic Venous Insufficiency
The primary cause of CVI is the dysfunction of venous valves and the weakening of vein walls, which can be influenced by genetic, environmental, and lifestyle factors. Congenital valve defects may predispose individuals to develop CVI, although acquired factors are more common. Damage to the veins’ structure often results from previous deep vein thrombosis (DVT), trauma, or inflammation that weakens the vessel walls and compromises valve function.
Age is a significant risk factor, as veins tend to lose elasticity and become less efficient over time. The natural aging process contributes to the deterioration of venous valves, increasing the likelihood of blood pooling in the legs. Additionally, women are more frequently affected, partly due to hormonal influences such as pregnancy and hormonal therapy, which can relax vein walls and valves. Pregnancy itself puts additional pressure on the veins, increasing the risk of developing CVI during and after gestation.
Occupational and lifestyle factors also play a crucial role. Jobs that require prolonged standing or sitting can impede normal blood flow, leading to venous hypertension. Sedentary lifestyles, obesity, and lack of physical activity contribute to poor circulation and increased venous pressure. Obesity adds extra weight and pressure on the lower limbs, aggravating the strain on veins and valves, thereby elevating the risk of CVI.
Genetic predisposition is another important factor, with a family history of venous disorders increasing susceptibility. Certain connective tissue disorders that weaken vessel walls can also contribute to the development of CVI. Additionally, smoking has been linked to vascular damage and impaired circulation, further heightening risk factors for venous insufficiency.
Overall, CVI results from a combination of intrinsic vessel wall weakness and extrinsic factors that impair venous return. Recognizing these causes and risk factors allows for targeted prevention efforts and early intervention, reducing the likelihood of progression to more severe venous disease.
Common Symptoms and Signs of Chronic Venous Insufficiency
Individuals with CVI often experience a range of symptoms that can vary in intensity and presentation. The most common early sign is leg swelling, particularly after prolonged periods of standing or sitting. This swelling, known as edema, results from blood pooling in the lower extremities due to impaired venous return. The swelling may improve with leg elevation, indicating venous involvement.
Another prominent symptom is the appearance of varicose veins—twisted, enlarged, and bulging veins that are visible beneath the skin. These veins often cause discomfort, heaviness, or a burning sensation in the legs. Patients may also notice skin discoloration, especially a brownish pigmentation around the ankles, which indicates chronic venous stasis and hemosiderin deposition from red blood cell breakdown.
Patients frequently report a sensation of aching, throbbing, or fatigue in the legs, which tends to worsen as the day progresses. Itching or dermatitis may occur due to skin inflammation and irritation caused by venous hypertension. In advanced cases, skin changes such as thickening, dryness, and ulceration can develop, particularly around the ankles. These ulcers are often painful, slow to heal, and prone to infection if not properly managed.
Other signs include muscle cramps, restless legs, and a feeling of fullness or pressure in the calves. Some individuals may also experience skin ulcerations or open sores, which are a hallmark of severe CVI. The presence of these signs typically indicates chronicity and potential progression of the disease, emphasizing the importance of early detection and management.
Recognizing these symptoms allows healthcare providers to differentiate CVI from other vascular or musculoskeletal conditions. Timely identification of signs and symptoms is crucial for initiating appropriate treatment strategies to alleviate discomfort, prevent complications, and improve overall quality of life.
Diagnostic Methods Used to Identify Venous Insufficiency
Diagnosis of Chronic Venous Insufficiency primarily relies on clinical evaluation and patient history. Healthcare providers assess symptoms such as leg swelling, varicose veins, skin changes, and discomfort. A thorough physical examination includes inspecting the skin for discoloration, ulcers, and signs of inflammation, as well as palpating veins for tenderness or enlargement.
Duplex ultrasonography is the gold standard diagnostic tool for CVI. This non-invasive imaging technique combines traditional ultrasound with Doppler flow assessment to visualize vein structure and evaluate blood flow dynamics. It helps identify venous reflux, valve incompetence, and vein obstructions, providing detailed information about the severity and extent of venous disease.
Venous filling and tourniquet tests can be performed as simple bedside assessments to evaluate venous competence. These tests involve observing the filling of veins after limb elevation or applying external pressure, which can indicate the presence of reflux or valve failure. However, they are less precise than duplex ultrasound.
In some cases, additional imaging such as venography may be employed, especially when surgical intervention is considered or if ultrasound results are inconclusive. Venography involves injecting contrast dye into the veins and taking X-ray images to visualize venous anatomy and detect obstructions or anomalies.
Laboratory tests are generally not specific for CVI but may be used to rule out other conditions such as deep vein thrombosis, infection, or systemic causes of edema. Overall, a combination of clinical assessment and duplex ultrasound provides the most accurate diagnosis, guiding appropriate treatment planning.
Accurate and early diagnosis of CVI is vital to prevent disease progression and complications. Regular monitoring and follow-up assessments help evaluate treatment effectiveness and adjust management strategies as needed.
The Role of Lifestyle Changes in Managing Venous Insufficiency
Lifestyle modifications play a fundamental role in managing Chronic Venous Insufficiency and preventing its progression. One of the most effective strategies is regular physical activity, such as walking or swimming, which stimulates calf muscle contractions and promotes venous return. Maintaining a healthy weight reduces pressure on the veins and alleviates symptoms.
Elevating the legs above heart level several times a day facilitates venous drainage and decreases swelling. Patients are advised to take breaks from prolonged standing or sitting, shifting positions frequently to encourage blood flow. Wearing compression stockings is another cornerstone of conservative management; these garments exert graduated pressure on the legs, supporting vein walls and improving circulation.
Dietary adjustments, including a balanced diet rich in fruits, vegetables, and low in salt, help control weight and minimize fluid retention. Avoiding excessive salt intake reduces edema and eases the burden on venous systems. Smoking cessation is also recommended, as smoking impairs vascular health and exacerbates venous problems.
Additional lifestyle tips include avoiding tight clothing around the waist or legs, which can impede blood flow, and managing underlying conditions such as hypertension or diabetes that may worsen venous health. Patients are encouraged to monitor their symptoms and seek medical advice when necessary.
Implementing these lifestyle changes can significantly improve symptoms, enhance venous function, and reduce the risk of developing complications. Education and support from healthcare providers are essential to motivate and sustain these habits over the long term.
Medical Treatments and Interventions for Chronic Venous Insufficiency
When conservative measures are insufficient, medical treatments are employed to manage CVI effectively. Compression therapy remains a mainstay, with graduated compression stockings designed to improve venous return and reduce edema. These stockings are available in various compression levels and should be fitted properly for maximum benefit.
Pharmacological options include venoactive drugs, such as flavonoids and horse chestnut extract, which aim to strengthen vein walls, reduce capillary permeability, and alleviate symptoms like leg heaviness and swelling. However, their efficacy varies among individuals and should be used as adjuncts to other treatments.
Endovenous procedures, such as sclerotherapy